A Nation's Obligation: Understanding the Veteran Suicide Crisis
- Security Halt Podcast

- 3 hours ago
- 9 min read
By Deny Caballero
Every single day in America, 17.5 Veterans die by suicide. Nearly one per hour. Not a statistic — 17.5 families. 17.5 sets of dog tags. 17.5 empty chairs at dinner tables across a country that owes these people everything.
The Department of Veterans Affairs' 2025 National Veteran Suicide Prevention Annual Report delivers the most comprehensive data ever compiled on suicide among the nation's 18.2 million Veterans. Drawing on death certificate records spanning 2001 through 2023, it reveals a crisis that has deepened significantly over two decades — and illuminates the populations, conditions, and circumstances at its heart.
This post breaks down the report's most critical findings, with particular emphasis on one of the most urgent and underrecognized connections in Veteran health: the documented link between traumatic brain injury and suicide risk.
6,398 Veteran suicide deaths in 2023 | 35.2 Suicides per 100,000 Veterans (up from 23.2 in 2001) | 73.3% Of Veteran suicides involved a firearm |
The Scale of the Crisis
In 2023, the Veteran suicide rate of 35.2 per 100,000 was more than double the non-Veteran adult rate of 16.9 per 100,000. Over the full 22-year span of the report, the age-adjusted rate increased 64.1% for female Veterans and 69.3% for male Veterans — compared to 41.0% and 11.7% respectively among their non-Veteran peers.
This happened against a shrinking Veteran population. There are roughly 7.7 million fewer Veterans alive today than in 2001. When the population contracts but the death count remains near 6,400 per year, it means the underlying risk is rising sharply. Veteran suicide claimed more American lives in 2023 than the entire Iraq War did across two decades of combat. It is the second leading cause of death for Veterans under 45.
Who Is Most at Risk
Young Veterans
Veterans aged 18 to 34 carry the highest suicide rate of any Veteran age group: 47.9 per 100,000 in 2023. The gap between young Veterans and their civilian peers is wider than at any other age. The transition out of the military is one of the highest-risk windows — characterized by identity disruption, loss of unit cohesion, reduced structure, and sudden disconnect from the mission that gave daily life meaning.
Female Veterans
Female Veterans face a crisis that receives far too little attention. After age adjustment, their 2023 suicide rate was 103.1% higher than for female non-Veterans — more than twice as high. Their firearm suicide rate was 168.3% higher than for female non-Veteran adults, and rose to 49.0% of female Veteran suicides in 2023, up from 45.3% the year before. From 2022 to 2023, female Veteran rates rose 2.8% while female non-Veteran rates fell 0.8%. The divergence is accelerating.
Geography: Where Risk Is Concentrated
Nevada leads all states in suicide rate at 61.2 per 100,000, followed by Utah (59.5), Oklahoma (56.9), West Virginia (55.6), and Montana (53.9). These are largely rural, Western states — which tracks with another consistent finding: rural Veterans have higher rates than urban Veterans, 45.1 versus 38.9 per 100,000. Geographic isolation, limited mental health infrastructure, and cultural norms around self-sufficiency all compound risk far from urban VA centers.
The Hidden Wound: Traumatic Brain Injury and Suicide
Of all the risk factors documented in the 2025 report, one demands urgent, immediate attention from the Veteran community, military families, clinicians, and Congress alike: the relationship between traumatic brain injury and suicide. It is one of the clearest, most consistent signals in two decades of data — and it is still not receiving the resources it requires.

Why TBI Raises Suicide Risk
Traumatic brain injury is not a simple physical injury. The neurological consequences of blast exposure, concussion, and penetrating head trauma can fundamentally alter the brain's architecture — damaging the regions responsible for impulse control, emotional regulation, decision-making, and the capacity to experience hope or pleasure. These are not abstract deficits. They are direct neurological pathways to suicidal crisis.
What makes TBI especially dangerous in the suicide context is the cascade of compounding consequences it triggers. Veterans living with TBI frequently face chronic pain, severe sleep disruption, cognitive difficulties, PTSD, and depression — each of which is itself an independent suicide risk factor. The report's Behavioral Health Autopsy Program findings, which analyzed the actual circumstances of Veteran suicide deaths from 2021 to 2023, show how these factors cluster:
• Pain was present in 52.3% of Veteran suicide cases reviewed — the single most common risk factor
• Sleep problems were present in 51.5% of cases
• Increased health problems in 43.1%
• Recent decline in physical ability in 34.8%
• Hopelessness in 30.2%
• Impulsivity or poor self-control in 24.9%
• Unsecured firearms in the home in 24.4%
Every item on that list is elevated in Veterans living with TBI. This is not coincidental. It is the documented, compounding effect of neurological damage meeting unmanaged pain, fractured sleep, broken relationships, and access to firearms — in a person whose brain has been compromised in its ability to regulate the impulse toward self-harm.
Twenty Years of Consistent Signal
The 2025 report documents Veteran suicide rates by TBI diagnosis status across every year from 2001 to 2023. In every single year without exception, Veterans with TBI diagnoses had significantly higher suicide rates than those without. This is not a recent trend or a statistical artifact. It is a two-decade pattern that the data has been shouting at us for years.
From 2001 to 2023, TBI diagnosis prevalence among VHA patients increased more than fourfold — from 0.64% to 2.8%. That growth reflects both improved diagnostic awareness and the lasting legacy of more than two decades of combat operations in Iraq and Afghanistan, where improvised explosive devices made blast-related TBI one of the signature wounds of an entire generation of service members.
IEDs were designed to kill. For the tens of thousands of Veterans who survived them, those devices left invisible damage that is still claiming lives today — not on the battlefield, but at home, years or decades later, often in ways that families never see coming until it is too late.
The TBI-to-Suicide Pipeline

What Integrated TBI Care Must Include
The evidence from the autopsy program and risk data is clear: suicide prevention for Veterans with TBI cannot be limited to psychiatric care alone. Effective programs must simultaneously address the complete picture of what TBI does to a human life.

The Twenty Highest-Risk Veteran Populations
The 2025 report identifies twenty Veteran subpopulations in VHA care with particularly elevated suicide rates. These are the communities where targeted outreach and intensive care coordination can save the most lives.

Mental Health Treatment: Progress and Persistent Gaps
Among Veterans in VHA care who died by suicide in 2023, 60.9% had a documented mental health or substance use disorder diagnosis in the prior year. That means 39.1% did not — nearly four in ten Veteran suicides among VHA patients occurred outside the mental health system's awareness. The safety net must reach further than clinical diagnosis.
The long-term trend for those inside the system is meaningfully encouraging. The suicide rate among Veterans with mental health or substance use diagnoses fell 34.7% from 2001 to 2023. Specific diagnosis groups saw even larger reductions: depression down 43.9%, anxiety disorders down 40.4%, PTSD down 34.9%. Treatment, delivered consistently over time, demonstrably prevents deaths.
Rising rates in other groups demand attention. Suicide rates increased for Veterans with other psychoses (+79.7% since 2001), cocaine use disorder (+57.0%), and amphetamine use disorder (+28.7%). The stimulant crisis among Veterans is real and growing.
The Physical Health Reality
Perhaps the report's most paradigm-shifting finding comes from the Behavioral Health Autopsy Program: when clinicians examined the actual circumstances of Veteran suicide deaths, the dominant risk factors were not psychiatric diagnoses — they were physical suffering and life disruption. Pain (52.3%), sleep problems (51.5%), worsening health (43.1%), physical decline (34.8%), and financial loss (23.6%) topped the list.
This is the picture of a body breaking down. A person who cannot sleep, cannot manage pain, has watched their physical ability diminish, and is running out of money. Suicide prevention that focuses exclusively on mental health diagnosis while ignoring these dimensions will continue to miss a substantial portion of those most at risk.
Special Populations Requiring Targeted Response
Homeless Veterans
Homeless Veterans in VHA care had a 2023 suicide rate 146% higher than non-homeless Veterans — a gap that has grown from 72.5% in 2001. Veterans with homelessness diagnoses who received VA homeless program services had a 33.7% lower rate than those without services. Housing is a suicide prevention intervention. Full stop.
Justice-Involved Veterans
Veterans in VHA care with justice program contacts had a 2023 rate of 144.6 per 100,000 — 263.7% higher than Veterans without justice involvement. The Veterans Justice Outreach program exists precisely to reach this population at the intersection of legal crisis, mental health, substance use, and housing instability.
Priority Group 5 Young Veterans
Veterans with income-based eligibility (no service-connected disability) have carried the highest suicide rate of any VA priority group for nearly every year since 2005. Among Priority Group 5 Veterans aged 18 to 35, the rate reached 85.4 per 100,000 in 2023 — a 37.9% increase in a single year. Economic stress is a suicide risk factor, and these Veterans are carrying that stress without a disability rating to help bear it.
Military Sexual Trauma
Veterans with positive MST screens had suicide rates 45.3% higher (female) and 27.6% higher (male) than those with negative screens. From 2022 to 2023, however, those rates fell 25.1% for women and 26.0% for men. Something is working for this population — and understanding what is working and scaling it should be an immediate research and policy priority.
What the Data Shows Us About What Works
This report is not solely a catalog of tragedy. Across 22 years of data, it documents genuine evidence that specific interventions save lives at measurable scale. These are not theoretical — they are documented in mortality statistics.
VHA Engagement Is Protective
The clearest policy signal in the entire report: Veterans who receive VHA care have seen suicide rates rise significantly more slowly than Veterans who do not. From 2001 to 2023, age-adjusted rates for male Veterans with VHA care rose 23.0% — compared to 71.1% for male Veterans without VHA care. For female Veterans, 29.6% versus 64.6%.
Veterans outside VHA care are experiencing roughly three times the relative rate increase. The system is frustrating and bureaucratic and imperfect. But the mortality data argues that being connected to VHA care is a meaningful protective factor — and that helping unconnected Veterans navigate enrollment should be treated as a life-saving mission, not an administrative nicety.
Mental Health Treatment Has Delivered Major Results
Over two decades, suicide rates for Veterans with depression diagnoses fell 43.9% within VHA care. For anxiety disorders, 40.4%. For PTSD, 34.9%. For alcohol use disorder, 16.3%. These are large, sustained reductions in some of the highest-risk populations in the country. The data demonstrates that evidence-based mental health treatment, delivered consistently over time, saves Veteran lives.
The Veterans Crisis Line Is Improving
Veterans who contact the Veterans Crisis Line are already in acute crisis — the 30-day post-contact suicide rate of 718.4 per 100,000 reflects the severity of their circumstances at the moment of contact. But the trend line is moving in the right direction. That 30-day rate is 24.2% lower than in 2019. The 12-month post-contact rate fell 16.1% from 2021 to 2022. Intensive crisis response and post-crisis follow-up care are measurably keeping Veterans alive.
Transition Support Is Making Incremental Gains
Veterans who separated from active duty in 2022 had the lowest 12-month post-separation suicide rate since 2016: 41.2 per 100,000, down 19.6% from the 2019 peak. This reflects improvements in pre-discharge mental health screening and transition support programming. The number remains dangerously high — particularly for those with pre-existing substance use disorders (152.6) or suicidal ideation history (130.7) — but the directional movement is encouraging.
Hormone Therapy: An Underreported Success
Among female Veterans aged 40 to 64 in VHA care who received menopausal hormone therapy, the suicide rate fell 54.7% over a twenty-year period — from 30.8 per 100,000 in 2004-2007 to 13.9 per 100,000 in 2020-2023. Among those who did not receive hormone therapy, the rate rose 18%. Whole-person health care, including hormonal health for women, has measurable suicide prevention effects. This finding deserves far more attention than it has received.
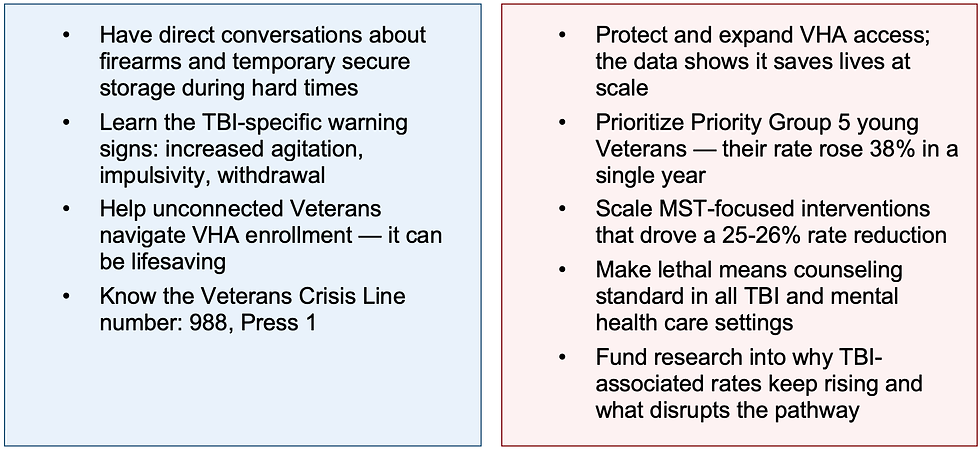
A Call to Action

The Bottom Line
The 2025 National Veteran Suicide Prevention Annual Report does not offer easy answers. The Veteran suicide crisis is real, multifaceted, and growing in critical populations. But 22 years of data also show us, clearly and consistently, that interventions work. That treatment works. That housing works. That community connection works. That access to VHA care works.
And for the tens of thousands of Veterans living with the invisible damage of traumatic brain injury — the message from the data is urgent and unambiguous: TBI is a major, documented, two-decade-long suicide risk factor. We have known this. The data has told us, every single year. What we owe these Veterans is action that matches the urgency of the evidence.
6,398 Veterans in 2023. 17.5 per day. Every one of them had a name, a history, and people who needed them to come home.











Comments